Is the increasingly rare instance of fully physician-led emergency medicine care teams crucial when the alternative is no care at all? Here’s why we believe well-trained APPs are closing the gap.
Providing a Pathway to Emergency Care in a Challenging Time
Without a doubt, 2023 was a year of shifts and challenges in the world of healthcare. Among the complex questions that hospital leaders and providers continue to contend with is: How do we adequately staff emergency departments amid the ever-looming physician shortage— whilst not sacrificing the standard of care? Though the specialized training of EM physicians remains unparalleled in value, the reality is that there are limited providers available. Some reports predict that the shortage will only continue to worsen, potentially not peaking until 2035.[i]
Nowhere are these staffing concerns more salient than in rural areas, which have seen unabated hospital closures across the nation.[ii] To respond to the mismatch of physicians available to work in rural communities and care demands, Aligned Providers Wyoming (APW) has committed to aiding partner hospitals with a sustainable solution: an advanced practice provider (APP) model that meets the highest level of quality and oversight.
As an independent, provider-owned group, APW is here to empower hospital leaders and clinicians to deliver the best care possible.
As an independent, provider-owned group, APW is here to empower hospital leaders and clinicians to deliver the best care possible. In this blog, we will give an overview of the emergency medicine staffing challenges that make it more vital than ever to develop creative staffing models. We will also introduce our own APP training program, which has proven successful in yielding positive outcomes for rural and underserved communities alike.
Feeling the Impacts of Bankruptcies, Closures, and the NSA
A complex set of factors impacted the business of emergency medicine in 2023. First, there was the bankruptcy and restructuring of one of the largest physician staffing groups– Envision Healthcare. Then there was the abrupt closure of another large staffing and management company, American Physician Partners. These disruptions amplified pressures on Envision and APP’s hospital partners and the clinician teams at their partner sites, making for unstable environments in which to run emergency departments and deliver care.[iii]
Meanwhile, the continued influence of the No Surprises Act (enacted in 2020 and implemented in 2022), which aimed to protect patients from unforeseen medical bills, had numerouse downstream impacts, including lower professional fees and more complex revenue cycle management tasks for emergency medicine groups. “This new reimbursement landscape has had a big impact on emergency medicine groups,” stated revenue cycle management expert Dr. Andrea Brault in a recent article.
Given requirements to see all patients, EDs have less flexibility in their business model, even when shifts in reimbursement rates cause reductions in revenue. Accordingly, shifts in rates have particularly affected “independent group practices or those in rural or underserved communities who are more sensitive to cash flow issues.”[iv] There’s some initial evidence that EDs are experiencing a close to 30% reduction in reimbursements for high-acuity cases in particular.[v]
Navigating the Ongoing Physician Shortage
Of today’s top hospital leadership challenges, staffing tops the list. It’s well known that the pandemic put a huge strain on medical professionals, causing an exodus of providers that the industry has still not recovered from. For those who stayed following COVID, a sense of fatigue and even moral injury pervade.
According to the AAMC, “emergency physicians and their fellow frontline clinicians have experienced a difficult few years, from the financial impacts of lower volumes early in the pandemic, to the burnout associated with the high volumes of the pandemic peaks, to the current challenges posed by nursing shortages leading to patients staying in the emergency department longer before hospital admission.”[vi]
In a recent Scientific American piece, “Fewer Physicians Are Choosing to Go Into Emergency Medicine,” the author (herself a physician) notes that in the last two years, the number of applications for usually competitive emergency medicine residencies has dropped by 26 percent. This is influenced not only by burnout but by the industry-specific stress of the business of emergency medicine itself. “The uncertainty of having to think on our feet that initially fueled our adrenaline has morphed into an uncertainty of staffing and resources that now fuels our anxieties,” she says. [vii]
“The uncertainty of having to think on our feet that initially fueled our adrenaline has morphed into an uncertainty of staffing and resources that now fuels our anxieties.”- Dr. Janice Blanchard, ER physician
Patients are certainly feeling the resulting distress. In a recent ACEP survey of 2,100 patients, 43% said they would “delay or avoid emergency care altogether due to concerns they would be held in hospital emergency departments for extended periods of time while waiting for an inpatient bed to open up.” On average, patients reported that when they did have to go to the ER, they waited from 4 to 13 hours to be seen.[viii]
The Future of Rural Care Depends on Expanding APP Availability
Given these challenges, it makes sense that many health leaders are wondering, How do we safely care for patients when there are simply not enough EM physicians to go around? For rural and underserved hospitals, the concern is about survival: How do we keep our doors open?
According to a report issued by the Center for Healthcare Quality and Payment Reform (CHQPR), “more than 600 rural U.S. hospitals are at risk of closing due to their financial instability.” This amounts to more than 30% of the country’s rural hospitals. Of these, at least half are facing immediate closure.[ix]
CHQPR predicts that the issue will worsen — particularly for smaller rural hospitals that continue to battle rising costs and workforce shortages.[x] In “care deserts” where hospitals have closed, patients sometimes travel exorbitant distances to receive care: over 100, 200, even 500 miles. Currently, a shocking nearly 80% of rural U.S. counties are considered medical deserts.[xi]
“There are many people who don’t see a doctor or get healthcare on a regular basis, and when they are really sick, they go to the emergency room for their care,” says April Kapu, past president of the American Association of Nurse Practitioners. “It is definitely a need in rural health that we get providers out in every community,” Kapu says. APPs help “ease care deserts created by physician shortages and rural hospital closings.” [xii]
“There are many people who don’t see a doctor or get healthcare on a regular basis, and when they are really sick, they go to the emergency room for their care,” says April Kapu, past president of the American Association of Nurse Practitioners. “It is definitely a need in rural health that we get providers out in every community.”
The good news? Rural America is already doing this. In areas suffering from provider shortages, gaps are increasingly being filled by APPs. According to research on ED staffing between 2013-2019, there was a significant increase in the share of rural sites being staffed by advanced practice providers.[xiii]
Emergency Medicine Workforce by Geography, 2013-2019
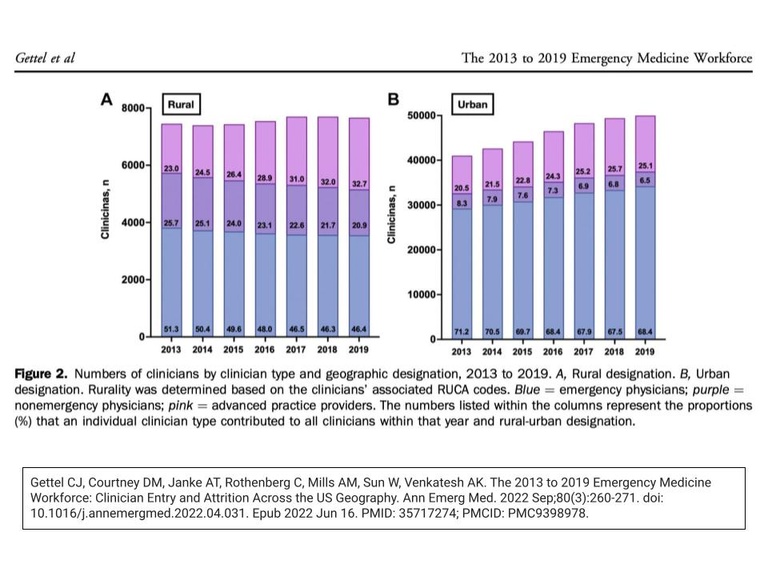
Source: Leon Adelman, Ivy Clinicians Blog 2023
As the dark pink portion of the rural graph illustrates, the numbers of APPs rose from 23.9 in 2013 to 32.7 in 2019. That’s an increase of 42% in six short years. While not as drastic, it’s worth noting that proportions of APPs in the urban sector rose in the same time frame as well.[xiv] Meanwhile, a different ACEP article reported that over the same time range, the “number of rural emergency physicians leaving the workforce was greater than the number of rural emergency physicians entering the workforce the following year.”[xv]
Independent billing trends reflect these shifts too. According to an article in Academic Emergency Medicine, 7.3% of high-acuity rural ED Medicare patients were billed independently by a physician assistant or nurse practitioner in 2013.[xvi] In 2019, approximately one in six (16.4%) rural high-acuity ED patients on Medicare were seen primarily by a PA or NP without being seen by a physician. This denotes a stunning 125% increase.[xvii] Over the same period, the portion of rural high-acuity Medicare patients seen by an emergency physician decreased from 74.5% to 66.6%.[xviii]
It should not be a surprise that APPs are independently billing and holding down the fort in rural emergency medicine, and doing it well. Nurse practitioners and physician assistants have long been crucially important players across the healthcare landscape, delivering treatment in the fields of neurology, intensive care, and more.
It is very common, for example, for an APP to receive a patient following an initial triage, conduct an examination, and create a treatment or discharge plan—consulting with an on-call physician via telemedicine (phone or video) in cases of more acute concern. APPs can also be trained at higher levels of life- and limb-saving procedures beyond what is offered at an urgent care or family practice.
This is exactly what we’re doing at Aligned Providers Wyoming, where we believe that cultivating talented APPs in the realm of emergency medicine is essential planning for the future. Our graduates are trained for an assortment of intensive procedures, including performing intubations (of both throat and chest), placing central lines, performing lumbar punctures, offering trauma care, and even performing cricothyrotomies. We train APPs to support care teams and even lead them (with the help of off-site supervision).
That said, we understand there are concerns about patient care quality when moving away from a physician-led ED model. Among the top-voiced issues are inexperience, quality, and cost. There is no doubt about the incredible value and specialized experience an EM physician provides.
However, when it comes to planning for the future of healthcare in rural communities with limited resources, the question needs to be asked: Is the increasingly rare instance of fully physician-led EM care preferable when the alternative is no care at all? Or can utilizing highly-trained advanced practice emergency medicine providers close the gap by offering a life-sustaining alternative in what would otherwise be another care desert?
Is the increasingly rare instance of fully physician-led EM care crucial when the alternative is no care at all? Or can utilizing highly-trained advanced practice emergency medicine providers close the gap by offering a life-sustaining alternative in what would otherwise be another care desert?
Luckily healthcare leaders don’t need to make that difficult choice. There is another way. Aligned Providers Wyoming has built an innovative APP training program that has dedicated itself to staffing hospitals with advanced practice providers to lead healthcare delivery in underserved areas.
Using the APP Model for Success at Aligned Providers Wyoming
APW is based in Wyoming, which has historically struggled with recruitment and staffing of medical talent. However, when our founders started APW, they had a vision for tapping into their decades of experience in multiple disciplines and across different geographies. Specifically, they wanted to train advanced practice providers to work and lead independently, treating high-acuity patients. That is exactly what APW has done.
Since APW started in 2016, we’ve unfortunately seen many struggling budgets and subsequent hospital closures in Wyoming. We’ve also seen what living in care deserts does to the rural families and communities affected. For example, we’ve seen the impacts on expectant mothers who don’t get proper prenatal care, or children who go untreated for strep throat, COVID, or even a broken bone.
In particular, we’ve seen hardworking members of the community – farmers, ranchers, and more—wait to get care because they couldn’t afford to take off a day of paid work to drive hundreds of miles for an appointment. “For many patients, time is their most precious commodity,” says Joann Bourlier-Childress, director of APPs at APW. “And they can’t afford to lose it.”
But unfortunately, delaying care denotes worsening outcomes for treatable issues, which then become emergent. This includes the cough that turns into pneumonia, the headache that precedes a stroke, or the heart attack that without timely care, becomes fatal. For all of these reasons, and to fulfill APW’s mission, we knew we wanted to expand the reach of our qualified APPs beyond Cheyenne. We wanted to help rural areas that would benefit from our deep experience across a variety of acuity levels.
For all of these reasons, and to fulfill APW’s mission, we knew we wanted to expand the reach of our qualified APPs beyond Cheyenne. We wanted to help rural areas that would benefit from our deep experience across a variety of acuity levels.
As previously noted, we trust our APPs to take on leadership roles because patient safety is so central to APW’s training program. Our commitment starts with an intensive vetting process for candidates. Once admitted, we teach students critical care procedures, and regularly test their competencies. Our 6- and 12-month APP internships feature 30 hours a week of clinical training, with an additional 10 hours a week of classroom instruction.
APW’s seasoned instructors equip interns with knowledge of both simple and advanced procedures to prepare them for ACLS/PALS/ATLS certification. Practitioners receive 1-1 attention, becoming well versed in responding to high-stress emergency situations and implementing acute interventions. Upon completing the program, our APPs go through an intensive sorting practice to best place them in the field.
What we’ve found since starting the training program is that an advanced practice provider model can ensure coverage, lower costs, and even improve patient experience. As leaders of rural hospitals know, it is more important than ever to open pathways to care. We believe in doing so responsibly and always adhering to the highest standard of excellence.
Read our next blog to learn about the steps we take to staff high-quality practitioners that can be depended on by rural communities, emergency medicine physicians, and hospital leaders alike. See how your organization can benefit from the same standard of excellence that made one of our partnering hospital leaders say, “I can’t believe how amazing that APP is. Do you have anyone else with her skill set?”
Endnotes
[i] https://time.com/6199666/physician-shortage-challenges-solutions/
[ii] https://medcitynews.com/2023/07/rural-hospital-insurance-finance/
[iii] https://emworkforce.substack.com/p/state-of-the-us-emergency-medicine
[iv] https://revcycleintelligence.com/news/unpacking-the-no-surprises-act-its-impact-on-emergency-medicine
[v] https://edpma.org/wp-content/uploads/2023/02/EDPMA-Data-Data-Analysis-No-Suprises-Act-FINAL.pdf
[vi] https://www.aamc.org/news/end-covid-19-public-health-emergency-could-further-strain-emergency-departments
[vii] https://www.scientificamerican.com/article/fewer-doctors-are-choosing-to-go-into-emergency-medicine/
[viii] https://www.beckershospitalreview.com/care-coordination/why-nearly-half-of-americans-avoid-emergency-care-new-acep-findings?utm_campaign=bhr&utm_source=website&utm_content=related{Footnote}
[ix] https://medcitynews.com/2023/07/rural-hospital-insurance-finance/
[x] https://medcitynews.com/2023/07/rural-hospital-insurance-finance/
[xi] https://www.healthleadersmedia.com/nursing/why-nurse-practitioners-are-solution-rural-healthcare-challengesFootnote
[xii] https://www.healthleadersmedia.com/nursing/why-nurse-practitioners-are-solution-rural-healthcare-challengesFootnote
[xiii] https://www.ivyclinicians.io/blog/42-percent-increase-in-app-share-of-rural-us-em-clinician-workforce-2013-2019/view
[xiv] https://www.ivyclinicians.io/blog/42-percent-increase-in-app-share-of-rural-us-em-clinician-workforce-2013-2019/view
[xvi] https://onlinelibrary.wiley.com/doi/10.1111/acem.14625?utm_source=newsletter&utm_medium=email&utm_campaign=Emergency+Medicine+Workforce+Newsletter&utm_id=More+high-acuity+ED+patients+are+being+seen+by+PAs+%26+NPs
[xvii] https://drive.google.com/file/d/1HqTb5VdOUnmsV5HpQB4QNhc1k0u6KTlY/view?utm_id=More+high-acuity+ED+patients+are+being+seen+by+PAs+%26+NPs
[xviii]https://www.ivyclinicians.io/blog/more-high-acuity-ed-patients-seen-by-pas-and-nps/view

